Virtual Reality for the Management of Chronic Pain – The VIPA Study
Jordan Tsigarides(1), Vanessa Grove(1), Jacqueline Chipping(1), Susan Miles(1), Nicholas Shenker(2), Saber Sami(1), Alexander Macgregor(1)
(1)Norwich Medical School, University of East Anglia, Norwich, United Kingdom
(2)Addenbrookes University Hospital, Cambridge, United Kingdom
Introduction
Chronic pain is debilitating, prevalent and one of the most prominent causes of disability worldwide. Current non-pharmacological treatments for pain conditions such as Fibromyalgia Syndrome (FMS) are labour intensive to implement and not widely available, especially during the pandemic.
Virtual reality (VR) has shown promise in the management of pain in acute settings1 with improvements in pain reporting corresponding to reduced activity within the pain neuromatrix in fMRI studies2. However, studies of use in chronic pain are limited, including diverse groups of patients with widely different interventions.
The VIPA Study is investigating the impact of different VR characteristics on acceptability and pain through a set of feasibility studies in specific chronic pain cohorts. Here we report on the VR experience and influence on pain among patients with FMS.
Methods
Patients with FMS were recruited through outpatient clinics at the Norfolk and Norwich University Hospital. Four VR systems representing the spectrum of commercially available technologies were used by participants in a random order, for approximately five minutes each. The interactive VR experience used with each head-mounted display (HMD) was co-developed alongside industry partners (Orbital Global). Participants were immersed within a naturalistic environment, situated on a wooden boat travelling slowly along a calm river surrounded by trees and hills. The interactive element involved the user shooting targets that appear using handheld controllers.
Baseline questionnaires included the McGill pain questionnaire short form (MPQ-SF; total score: 0-45) and a pain visual analogue scale (VAS; 0-10). VAS data were also reported after use of each HMD. Subjective experience questionnaires collected data with 7-point Likert scale rating questions (1=strongly disagree to 7=strongly agree). The VR sickness questionnaire gained side-effect data (VRSQ; total severity score: 0-100). Likert-scale data were dichotomised (rating ≤3: disagree, rating ≥5: agree).
Results and Discussion
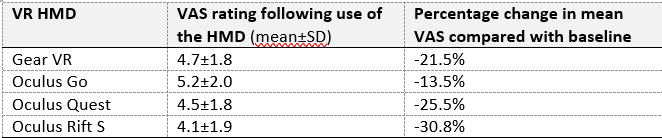
13 participants with FMS were included (mean age 41.8±15.6, 92.3% female) with moderate self-reported pain at baseline (mean MPQ 25.5±8.8, VAS 6.0±1.7). Only 30.8% had previous VR exposure. Across HMDs, side effects were mild and infrequent (average mean VRSQ 17.3±9.7). Participants reported reduced pain VAS scores following use of each headset compared to baseline (see table 1). Following use of the Oculus Rift S, 100% agreed that they felt immersed within the virtual world (mean rating 6.46±0.78) and 92% agreed that they had more attention for the experience than for their own thoughts (mean rating 6.54±0.88). 77% also agreed that they lost track of time whilst undergoing the VR experience (mean rating 5.85±1.46).
Table 1: VAS data following use of each VR HMD
Our results strengthen the rationale for use of therapeutic VR in chronic pain. FMS patients found VR immersive and engaging, favouring the Oculus Rift S. Patients reported significantly lower pain regardless of the HMD used, with minimal side effects. This feasibility work paves the way for a larger clinical trial investigating efficacy, dose-response and impact on medication use.
Conclusions
Therapeutic VR provides an accessible, non-pharmacological pain management option of the future with clear benefits over traditional approaches given its ability to be delivered in patients’ homes.
References
1. Dascal J, Reid M, Ishak WW, Spiegel B, Recacho J, Rosen B, Danovitch I. Virtual reality and medical inpatients: A systematic review of randomized, controlled trials. Innov Clin Neurosci 2017;14(1-2):14-21
2. Hoffman HG, Richards TL, Coda B, Bills AR, Blough D, Richards AL, Sharar SR. Modulation of thermal pain-related brain activity with virtual reality: evidence from fMRI. NeuroReport 2004;15(8):1245-8
3. Jones T, Moore T and Choo J. The impact of virtual reality on chronic pain. PLoS One 2016;11(12):e0167523